Herniated Disc Treatment Options for Relief
Updated:

Learn More About Slipped Disc & Back Pain Causes
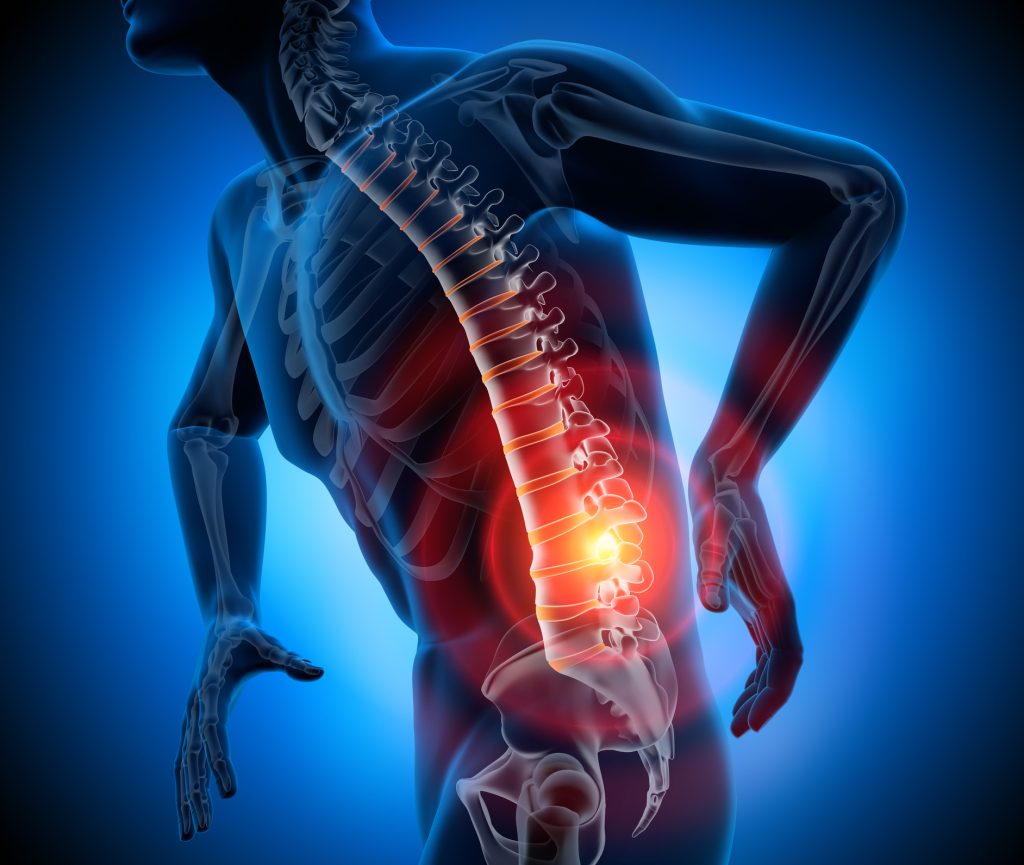
A slipped disc is an old-fashioned term that doesn’t truly describe what happens when somene experiences it. It’s more accurate to refer to it as a disc herniation, disc prolapse, or disc bulge. A herniated disc often causes a person to experience sudden and severe lower back pain. The disc puts pressure on a nerve, causing pain down one leg. In most cases, the symptoms gradually ease over a period of several weeks.
More than 3 million people in the U.S. suffer from a herniated disc each year. Herniated discs are the leading cause of neck, back, and leg pain and can happen anywhere along the spine. However, they most often occur in the lower back (lumber spine) or neck (cervical spine). Below, the experts at Spine Art review information about herniated discs, their associated symptoms, and common treatments. Reach out to our team to learn more about what we offer patients at Spine Art.
What Is a Herniated Disc?
In cases of a “slipped disc,” a disc does not actually slip out of place in your back. Two processes can be referred to as a slipped disc:
- Part of the inner part of the disc pushes out through a weakness in the outer part of the disc (herniated disc).
- In some cases, the outer layer of the disc bulges because its flexibility has decreased over time. This is referred to as a disc bulge.
In both cases, the bulging part of the disc may apply pressure to nearby nerves coming from the spinal cord. Inflammation can also develop around the prolapsed part of the disc. Inflammation may irritate a nerve and cause swelling, which may put pressure on a nerve. Any disc in the spine can prolapse. However, 95 of 100 prolapsed discs occur in the lower back (the lumbar spine). The size of a disc prolapse can vary. The larger the prolapse, the more severe the symptoms are likely to be. It’s common for a prolapsed disc or disc bulge to be detected on MRI scans in people with no symptoms at all.
Causes & Risk Factors
Disc herniation is typically the result of gradual, age-related wear and tear called disc degeneration. Our discs become less flexible and more prone to tearing with even the most minor strain as we age. Most people can’t pinpoint the cause of their herniated discs, but some causes include lifting heavy things improperly or twisting and turning while lifting. Traumatic events such as a fall or a blow to the back are rarely the cause of herniated discs. Several factors can increase the risk of getting a herniated disc, including:
- Weight: Excess body weight causes stress on the discs in the lower back.
- Occupation: If you have a physically demanding job, you have a greater risk of experiencing back problems. Repetitive lifting, pushing, pulling, bending, and twisting can also increase the risk of getting a herniated disc.
- Genetics: Some people have a predisposition to developing a herniated disc due to their genetics.
- Smoking: Smoking lessens the oxygen supply to discs, causing them to deteriorate more quickly.
- Frequent Driving: Sitting for long periods can put pressure on the spine.
- Being Sedentary: Participating in regular physical activity can help prevent a herniated disc.
What are the Symptoms of Herniated Disc?
Most herniated discs occur in the lower back, but they also can occur in the neck. Symptoms depend on where the disc is sitting and whether the disc is pressing on a nerve. Herniated discs often affect one side of the body. Some common symptoms include the following:
- Arm or Leg Pain: If your herniated disc affects your lower back, you’ll typically feel pain in your lower back, buttocks, thigh, and calf. You might have pain in part of your foot as well. For a herniated disc in the neck, people usually experience the most pain in their shoulders and arms. The pain is often described by patients as sharp or burning.
- Numbness or Tingling: People with herniated discs often experience radiating numbness or tingling in the body part served by the affected nerves.
- Weakness: Muscles served by the compressed nerves tend to weaken, which can cause a person to stumble or have difficulty lifting things.
Diagnosis
Your healthcare provider will conduct a thorough physical examination to diagnose your condition. During the exam, they will assess your pain, muscle reflexes, sensation, and strength. They may refer you for a neurological exam and a straight leg raise test. Your provider may also order imaging tests, including the following:
- X-rays
- Myelogram
- Magnetic resonance imaging (MRI) scan
- Computed tomography (CT) scan
- Electromyogram (EMG)
- Nerve conduction study
Treatment Options
You may need more advanced herniated disc treatment if your symptoms aren’t improving. Your healthcare provider might recommend the following:
- Medication: Your provider may prescribe an anti-inflammatory pain reliever or muscle relaxant.
- Physical Therapy: A physical therapist teaches you a fitness program to help relieve pressure on your nerves. Physical activity loosens tight muscles and improves circulation.
- Spinal Injections: A spinal injection is a shot of steroid medication directly into your spine, called an epidural or nerve block.
In most cases, pain from a slipped disc can go away in time. To ease the pain while your disc heals, you can:
- Rest for one to three days if the pain is severe but avoid long periods of bed rest to prevent stiffness.
- Take over-the-counter pain relievers, like ibuprofen or acetaminophen.
- Switch off applying ice and heat to the affected area.
Surgical treatments can include Microdiscectomy (common surgery for herniated discs) and spinal fusion or artificial disc replacement (in severe cases)
Recovery & Lifestyle Adjustments
It’s not always possible to prevent a bulging disc. However, you can reduce your risk by:
- Using proper lifting techniques: Bend your knees while keeping your back straight when lifting heavy objects. Use your leg muscles to help support the weight.
- Maintaining a healthy weight: Excess weight puts pressure on your lower back.
- Practising good posture: Improve your posture when walking, sitting, standing, and sleeping. Good posture reduces strain on your spine.
- Stretching: Taking stretching breaks is essential if you often sit for long periods.
- Avoid wearing high-heeled shoes: This type of shoe causes spine misalignment.
- Getting regular physical activity: Focus on physical workouts that strengthen your back and abdomen muscles to help support your spine.
- Stopping smoking: Smoking can weaken discs, making them vulnerable to rupture.
Herniated Disc FAQs
A herniated disc can usually heal on its own, with most cases resolving within a few weeks to a few months through the body’s natural healing process, which involves the absorption of the herniated disc material and reduced nerve compression; however, the severity of the herniation and individual factors can influence the healing time and may require conservative treatments like rest, pain medication, and physical therapy to manage symptoms.
For the majority of patients, herniated disc pain improves on its own or with simple medical care. Most people feel better within four to six weeks. If your symptoms don’t improve, you should see a healthcare provider to determine the cause of the issue and develop a treatment plan. Some people require more aggressive medical measures, such as spinal injections or herniated disc surgery.
No, surgery is not always necessary for a herniated disc. Most people with a herniated disc can manage their symptoms without surgery. When surgery might be necessary:
– If symptoms get worse
– If symptoms have lasted at least six weeks
– If symptoms make it hard to do everyday activities
– If other treatments haven’t helped
– If you have extreme weakness in a leg
– If you have extreme and unmanageable pain
Initially, you can treat herniated disc pain at home. However, you should see a healthcare provider if:
– The pain interferes with your daily life, like driving and going to work.
– Your symptoms are worsening or aren’t improving after six weeks.
– You lack bladder or bowel control.
– You notice numbness, tingling, or weakness in your hands, arms, legs, or feet.
– You have difficulty standing or walking.
– Your neck or back pain travels down your arms or legs in combination with numbness, tingling, or weakness.
Contact Spine Art Today for Herniated Disc Treatment
Herniated discs are a manageable and treatable condition. If you think you’re experiencing the common symptoms of one, we recommend scheduling an appointment with a spine specialist to find the best treatment options. Spine Art aims to provide the best care possible for patients with degenerate or arthritic back pain, spondylotic neck pain, spinal stenosis, or other common problems such as a slipped disc causing sciatica or nerve root pain. Contact our team today to learn more about our spinal services and treatments.








